Oral Presentation Annual Meetings of the Endocrine Society of Australia and Society for Reproductive Biology and Australia and New Zealand Bone and Mineral Society 2016
Fractures in spina bifida from childhood to adulthood (#91)
Background: Fractures are common in children with spina bifida, with the distal femur being the predominant site of fracture. However, the literature examining site and rates of fracture in adulthood is scant.
Aims: To study the prevalence, type and risk factors for fracture according to age in spina bifida.
Methods Retrospective cohort study of 146 individuals with spina bifida aged 2-52 years who attended the spina bifida multidisciplinary clinic at a single tertiary hospital. Of the 77 adults, 47 had dual energy x-ray absorptiometry (DXA) performed. At the lumbar spine, bone mineral density (BMD) of L1 was assessed, as it is rarely deficient in spina bifida.
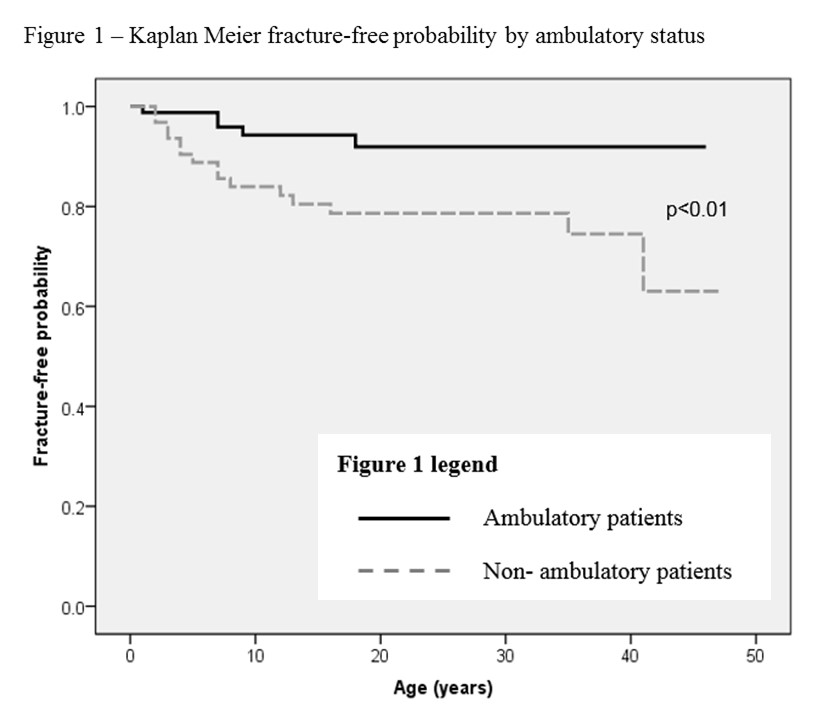
Results There were 32 fractures in 21 patients. Median age of first fracture was 7 years (interquartile range IQR 4-13yrs). Fracture rates in children, adolescents and adults were 10.9/1000 (95% confidence interval 5.9-18.3), 5.4/1000 (95% CI 1.5-13.8) and 2.9/1000 (95% CI 0.6-8.1) patient years, respectively. Childhood fractures predominantly involved the distal femur; these fractures were rarely seen in adulthood. Non-ambulatory status was associated with a 9.8 times higher risk of fracture compared with ambulatory patients (OR 9.8, p= 0.016, 95% CI 1.5-63.0) (Figure 1). Relative risk of re-fracture was 3.1 (95% CI 1.4-6.8). Median age of the 47 adults who underwent DXA was 32.7 years (IQR 22.3 – 39.0). There was discordance between hip and spine BMD with a median L1 Z-score of -1.3 (IQR -2.1 to -0.1) and median femoral neck Z-score of -2.1 (IQR -3.0 to -0.9). Areal BMD or BMD Z-scores at any site did not predict fracture.
Conclusions The risk of fracture is lower in young adults compared with children with spina bifida. Nevertheless, adult patients who are non-ambulatory or have a prior fracture are at increased risk and should be targeted for fracture prevention.